PATHOGENESIS:
Infection begins when T. pallidum penetrates the host, usually through intact or abraded mucous membranes; virulence factors: hemolysins, membrane proteins allowing for permeability of nutrients but inaccessible to antibody, ligands that allow cytoadhesion; the ensuing inflammation is responsible for most of the disease pathology. In the early disease, spirochetes can be found in the chancre, the usual first manifestation of syphilis. Invasion into the bloodstream and lymphatics occurs within hours to days of penetration of T. pallidum as evidenced by the fact that patients who received blood transfusions from syphilitic donors in the seronegative incubation period have become infected. All organs of the body can be invaded but the skin, lymph nodes, and the central nervous system (CNS) are the sites most often invaded. In the skin, T. pallidum is found in the dermal-epidermal junction zone or throughout the dermis.
Both humoral and cell mediated immune responses are mounted against T. pallidum. At all stages of infection, there are local cellular infiltrates consisting of lymphocytes, macrophages, and plasma cells at the sites of disease. In primary syphilis, CD4+ T cells and macrophages are the predominate cell type while in secondary syphilis CD8+ cells predominate. In both primary and secondary syphilis, there is increased expression of TH1 cytokines IL-2 and IFN-Gamma. Cell mediated and humoral immune responses peak in secondary syphilis. Spirochetes may remain alive and continue to replicate in immunologically sequestered sites in the body even with a brisk initial immune response and no outward clinical manifestations of disease in at least 1 of 4 persons who are not treated. In late latent syphilis, after many years of latency, treponemes begin to multiple and Th1 lymphocytes produce high levels of nitric oxide and IL-12 instead of Il-2 and IFN.
LABORATORY DIAGNOSIS:
- bacteriological - microscopic examination; pathological products from patient;
- serological - changes in the patient's serum; most known: VDRL (Venereal Disease Research Laboratory), Bordet-Wassermann reaction (first blood test for syphilis, nontreponemal category; RPR and VDRL replaced it).
T. pallidum lacks many pathways including the tricarboxylic acid cycle, components of oxidative phosphorylation and most biosynthetic pathways, and relies on the host to perform necessary functions.
Persons are most infectious early in disease when a chancre, mucous patch, or condyloma latum is present and by 4 years after acquiring the disease.
Clinical manifestations: traditionally divided into five stages: incubating, primary, secondary, latent (early latent and late latent), and late or tertiary syphilis (neurosyphilis, cardiovascular syphilis and gummatous syphilis).
Primary syphilis: 3 to 90 days (a median of 3 weeks) after infection. Single, painless chancre or ulcer develops at the site of inoculation. In some persons, it does not develop at all; in others, it is so small that it may go completely unnoticed. In those with HIV, multiple ulcers may develop.
Secondary syphilis: widespread dissemination to various parts of the body. It becomes evident in a mean of 6 weeks after inoculation. In 90% of cases, there is a rash which most commonly is widely disseminated, maculopapular and involves the palms and soles but other dermatological manifestations are also common. Over 50% of cases have fever, malaise, anorexia, weight loss, pharyngitis, laryngitis, and/or arthralgias. Other manifestations: lesions in the mouth and oral cavity, lymphadenopathy, condyloma latum, glomerulonephritis, nephritic syndrome, hepatitis, arthritis, osteitis, and periosteitis.
Latent syphilis is the period of months to years post infection in which there are no outward clinical manifestations of disease despite viable organisms. Clinical relapses can occur during the first year of the latent stage (referred to as the early latent phase), as a result of waning specific cellular immunity.
Tertiary/late syphilis: in up to 35% of untreated patients 10 to 25 years after the initial infection. Can be categorized into: neurosyphilis, cardiovascular syphilis and granulomatous syphilis. The latter 2: uncommon in the antibiotic (frequent antibiotics' exposure); neurosyphilis: most common manifestation of tertiary/late syphilis nowadays (generally poor penetration of antibiotics into the CNS).
A VARIETY OF LABORATORY TESTS HAVE BEEN DEVELOPED TO OVERCOME THE INABILITY TO CULTURE T. PALLIDUM USING STANDARD LABORATORY METHODS:
• DIRECT DETECTION METHODS
- not widely available; false negative tests relatively common (30%).
Dark Field Microscopy
- sensitive, direct, quick (in active lesions); specimens best obtained from serous transudate of moist lesions such as a primary chancre, condyloma latum or mucous patches (from dry skin or lymph nodes by non-bactericidal saline aspiration).
- under dark field microscopy, T. pallidum will appear as corkscrew shape in spiraling motion with a 90° undulation about its midpoint (3 or more specimens required before deciding for non-syphilitic).
Polymerase chain reaction (PCR)
- can detect T. pallidum genetic material, most often the PoIA gene; most commonly used to detect congenital syphilis, but also effective for primary syphilis.
Immunofluorescent and Immunoperoxidase Antibody Staining
- can be used to visualize nonviable spirochetes, from mucocutaneous lesions, lymph nodes, dry skin.
• SEROLOGICAL TESTS
Nontreponemal Reaginic Antibody Tests
Syphilis reaginic antibodies are IgG and IgM antibodies directed against a lipoidal antigen resulting from the interaction of host tissues with T. pallidum or from T. pallidum itself. VDRL slide test: first nontreponemal test developed; except for its use in diagnosing neurosyphilis, it has now been largely replaced by the modifications such as the rapid plasma reagin (RPR) card test, automated reagin test (ART).
Nontreponemal tests become positive shortly after initial infection, peak during the secondary or early latent stage, and then decline with time. In primary syphilis, an antibody response may not yet have been generated so nontreponemal tests may be negative. In secondary syphilis, virtually 100% of infected persons have positive serological tests for syphilis but in some patients the titers are so high that the test is reported as negative due to the prozone phenomenon. On the other hand, whenever there is a strong immunologic stimulus (e.g. acute bacterial or viral infection, vaccination, HIV infection), a "false" positive occurs. In addition, persons who use injection drugs, have autoimmune or connective tissue diseases (especially systemic lupus erythematosus), or hypergammaglobulinemic states may have "false" positive results. These persons often also have blood tests positive for other factors frequently associated with autoimmune disease such as antinuclear, antithyroid, or antimitochondrial antibodies; rheumatoid factor; and cryoglobulins. A negative specific treponemal test will confirm that the test is a false positive and that syphilis can be excluded.
Fluorescent Treponemal Antibody-Absorption (FTA-abs)
- uses T. pallidum harvested from rabbit testes as the antigen in a standard indirect immunofluorescent antibody test; confirms/refutes a positive nontreponemal test. At high suspicion, diagnoses syphilis even when a nontreponemal test is negative.
T. pallidum Haemagglutination Assay (TPHA) and Microhemagglutination Assay for Antibodies to T. pallidum (MHATP)
- TPHA measures specific treponemal antibody; performed easier than the FTA-abs and as specific, but not as sensitive, especially in early disease;
- MHATP is similar to TPHA, except it uses a microtiter plate; "sorbent" is always used to increase its specificity.
Enzyme-linked Immunosorbent Assay (ELISA)
- immunoassay detecting T. pallidum specific antibodies; may detect only IgG or IgM but most assays are polyvalent. As with all ELISAs, an enzyme is conjugated with anti-human antibodies and only those wells that contain T. pallidum specific antibodies conjugated to the enzyme will exhibit a color change. The sensitivity and specificity of ELISAs are similar to TPHA and FTA-Abs. Compared with the RPR and MHATP sensitivities, ELISA is more sensitive in all stages of syphilis except in secondary syphilis when all tests show 100% sensitivity.
Immunochromatographic Membrane Test (ICT)
- rapid test detecting T. pallidum antibodies employing anti-human immunoglobulins gold conjugate and highly purified TP recombinant proteins bound to a membrane; advantage over ELISA: it is visually read and can be performed at the point of care.
Immunochromatographic Strip (ICS)
- a "lateral flow" test in which antibodies in a specimen are detected by becoming bound to antigens, marked with dye, on a cellulose strip; like ICTs, it requires no special training to read, laboratory equipment to run, or refrigeration of reagents or samples.
Line immunoassay (LIA)
- uses recombinant and synthetic polypeptide antigens derived from T. pallidum proteins to determine if a clinical specimen has treponemal antibodies; like ICTs and the ICS test, it is inexpensive, rapid, and requires no special laboratory equipment or highly trained personnel.
INDICATIONS FOR LUMBAR PUNCTURE:
- any patient with symptoms and/or signs of neurologic or ophthalmic disease should have an evaluation that includes CSF analysis, ophthalmologic examination and otologic evaluation;
- patients whose symptoms and/or signs persist posttreatment for early syphilis or recur or who have four-fold increases in their NTA titers should be considered to be treatment failures or re-infected and all should have a lumbar puncture. Patients with latent syphilis who meet any of the following three criteria also should have lumbar punctures: patients whose symptoms and/or signs persist posttreatment for early syphilis or recur or who have four-fold increases in their NTA titers should be considered to be treatment failures or re-infected and all should have a lumbar puncture;
Changes consistent with syphilis in the CSF include the following:
- an elevated cell count usually of less than 200 cells predominantly lymphocytes
- elevated protein up to 200 mg/dL
- normal glucose in the majority of patients though it may be modestly decreased in about a third positive NTA test (TSAs are not used for the diagnosis of central nervous system syphilis)
Patients with abnormal spinal fluid results should have repeat studies performed at 6 month intervals until the cell count is normal. Elevated protein levels and the CSF NTA antibody titer may take longer to resolve and are not important as long as the CSF cell count returns to normal.
If cell counts have not returned to normal by 2 years the patient should be re-treated.
Keep in mind that HIV infection causes CSF pleocytosis and elevated protein levels independent of syphilis and this may be an explanation for nonresolution of CSF abnormalities in such persons.
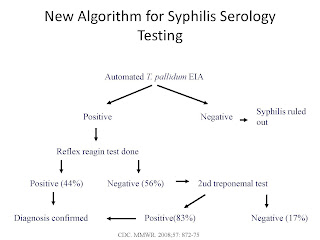
TESTING ALGORITHMS FOR SYPHILIS IN ADULTS EXCEPT NEUROSYPHILIS
Diagnosing syphilis algorithm: nontreponemal test; if reactive, verify with FTA-abs, TPHA, MHATP, or ELISA. If both tests are reactive, then a person is considered to have present or past syphilis infection. Treatment decisions are based on past history and nontreponemal titers.
As with the traditional method, when a person is reactive to both a specific treponemal such as a positive ELISA test and nontreponemal test such as a RPR, then a person is considered to have active disease requiring treatment. When a person is reactive to the treponemal test but nonreactive to the nontreponemal test such as a RPR test, persons with a history of previous treatment will require non further management. Those with no prior history of treatment should have a different treponemal test performed such as an FTA-abs. If the second test is also nonreactive, then the clinician needs to use his/her clinical judgement to decide whether or not a third treponemal test is indicated.
TESTING ALGORITHMS FOR CONGENITAL SYPHILIS
A lumbar puncture with the CSF sent for VDRL, cytology, and protein is the most commonly used method for making the diagnosis. A reactive CSF-VDRL is considered diagnostic of syphilis while a negative test does not rule out disease, e.g., it is a specific but not very sensitive test. If the CSF-VDRL is negative, a finding of >5 mononuclear cells per cubic millimeter, a protein value of ≥46 mg/dL, or a glucose of ≤45 mg/dL, all suggest neurosyphilis.
Methods with greater sensitivity and specificity than the CSF-VDRL are the intrathecal T. pallidum antibody (ITPA) and TPHA. A FTA-abs test is usually not performed on CSF because a positive test may represent passive transfer of antibody from serum to the CSF and not active CNS disease. However, it is highly sensitive and thus a negative test can be helpful in ruling out neurosyphilis, especially in HIV infected patients who often have white blood cells in the CSF.
SUSCEPTIBILITY IN VITRO AND IN VIVO
Penicillin, the first antibiotic developed, was the first known effective antibiotic for T. pallidum and remains the treatment of choice today. T. pallidum can regenerate if the serum penicillin concentration falls to sub-inhibitory levels for 24-30 hours.
T. pallidum is also susceptible to virtually all other β-lactam antibiotics (amoxicillin, ceftriaxone, ceftizoxime, cefmetazole, cefetamet). Macrolide antibiotics are also able to inhibit T. pallidum but not as efficiently as the β-lactam antibiotics.
Combination therapy for syphilis is no more efficacious than single drug therapy. The addition of amoxicillin and probenecid for 10 days to 2.4 million units of penicillin achieves similar result as penicillin alone.
CLINICAL PRESENTATION OF SYPHILIS
- can mainly be divided into early syphilis and late syphilis.
EARLY SYPHILIS
- primary syphilis: the primary ulcer or chancre: on the genitals, perianal skin, within the rectum, oral cavity, and any other skin or mucous membrane surface exposed to an infectious lesion that was present on the source sexual partner. The average incubation period is 3 weeks but can vary from 10 to 90 days. Any genital ulcer should be considered to be syphilis until proven otherwise. The lesions of primary syphilis will resolve within 3 to 6 weeks without treatment. Of course, the individual remains infected and will become infectious again with the advent of secondary syphilis.
- secondary syphilis: left untreated, the organism disseminates hematogenously from the site of the primary infection to all parts of the body. This occurs within a few weeks or months of the onset of the primary lesions. Cutaneous and/or mucous membrane lesions are the most common clinical manifestations of the phenomenon and occasionally the primary lesion persists.
Initially erythematous macules which evolve into hyperpigmented papules. Skin lesions are usually present on both the palms and soles and any rash with this distribution should immediately bring secondary syphilis to mind. Mucosal lesions are generally superficial, ulcerated, and painless with gray borders. Similar lesions may be found on the foreskin, penile head, and intravaginally. Patchy alopecia can be a manifestation of scalp involvement in secondary syphilis. Low grade fever, malaise, headache, and generalized lymphadenopathy often accompany dissemination.
Uncommon systemic manifestations of secondary syphilis include gastritis, mild hepatitis, and aseptic meningitis. As with the primary chancre, the manifestations of secondary syphilis also will resolve spontaneously over time but over a period of a few years there may be relapses of secondary disease.
- EARLY LATENT SYPHILIS: asymptomatic person with a normal physical examination who is diagnosed serologically and has a history of syphilis exposure within the preceding 1 year.
LATE SYPHILIS
- neurosyphilis
Persons who have syphilis and symptoms or signs suggesting neurologic or ophthalmic disease should have an evaluation that includes CSF analysis, ocular slit-lamp ophthalmologic examination, and otologic examination.
Acute syphilitic meningitis: The incubation period for this relatively rare syndrome is usually less than 1 year; treatment is the same as for late disease. Symptoms and signs of meningitis are the first clinical manifestations in only a quarter of patients.
In some of these patients the cerebrospinal fluid (CSF) examination is normal, particularly those with isolated 8th nerve disease, though the majority have modestly elevated cell counts, increased protein, and positive CSF serologic tests or a combination of these results.
Cerebrovascular syphilis: incubation period is 5 to 12 years after the initial infection. The most common manifestations are hemiparesis or hemiplegia. It affects the middle and anterior cerebral arteries most frequently. Other presenting problems include aphasia and seizures.
Neurosyphilis should be strongly suspected in all younger patients presenting with cerebrovascular accidents.
Ocular syphilis: have been reported increasingly; most suspected cases in males, half in HIV-positive persons. A significant proportion of cases have been reported in patients with early syphilis. Severe outcomes, including blindness, have been reported in both HIV-positive and negative patients.
All patients diagnosed with syphilis that exhibit ocular manifestations should immediately be treated for neurosyphilis and be referred for formal ophthalmologic examination. Optic atrophy in the absence of signs of inflammation may be found in association with other manifestations of neurosyphilis or may be an isolated finding of late syphilis.
Nonneurologic manifestations of late syphilis (tertiary syphilis): various cardiovascular diseases. Late benign syphilis lesions or gummas are rarely seen today.
What laboratory tests should you order and what should expect to find?
- A dark field examination of fluid expressed directly from a lesion in the time-honored diagnostic test for patients with the skin lesions of primary and secondary syphilis; the specimen is obtained by pressing a glass slide directly onto a lesion and then placing it immediately under a darkfield microscope for reading.
Serologic tests are the cornerstone of syphilis diagnosis. There are two general types of tests:
The reagin or nontreponemal assays (NTAs) is based on the fact that human antibodies induced by T. pallidum infection cross react with mammalian cardiolipin. In essence this is an "autoantibody" and therefore it is not too surprising that it lacks specificity. Conditions associated with false positive NTAs include old age, pregnancy, malignancy, and collagen vascular disease among others. The advantage of NTAs is the rise and fall of antibody titers reflect the course of disease including decreasing titers in patients who have been successfully treated. A four-fold reduction in titer over a period of 3 to 12 months is accepted as evidence of treatment success. An additional advantage is that one of the NTAs, the rapid plasma reagin (RPR) card agglutination test, is relatively quick and simple to perform.
The treponeme specific assays (TSAs) traditionally have been used to confirm that a positive NTA is a true positive test. Following this algorithm when a syphilis serology is ordered on a patient the laboratory first performs a NTA and if positive then automatically performs a TSA test to differentiate between a true and a false positive NTA result. The TSAs generally are more complex tests and take more time so in the case of a negative NTA they are not performed.
Interpretation of syphilis serologic assays following the traditional testing algorithm: neither a negative NTA nor negative TSA rules out primary syphilis. It follows then that in a patient suspected of having a primary chancre, if the RPR is negative the patient should be treated for primary syphilis empirically. Such patients can be invited to return to the clinic in several weeks to determine if seroconversion has occurred. In contrast to primary syphilis, a negative NTA almost does rule out secondary syphilis. Over a period of years following an untreated primary infection, the NTA test will become negative in a proportion of patients with late syphilis while the TSA remains positive in almost all cases. Therefore, if an NTA is negative in a patient suspected clinically of having late syphilis the care provider should order a TSA. Remember that the laboratory only performs this test automatically if the NTA is positive.
List of available serologic tests for syphilis (top below) and expected results of serologic testing in patients with untreated syphilis (bottom below):
TESTING GUIDELINES - SUMMARY:
TREPONEMA PALLIDUM (SYPHILIS) SCREENING CASCADE: